Definition
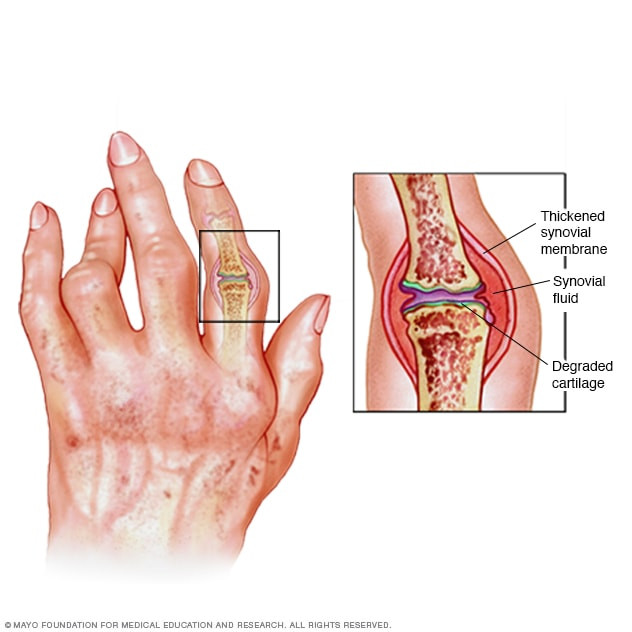
Psoriatic arthritis is a chronic (long-term) disease characterized by joint inflammation experienced by individuals with psoriasis. Symptoms can include joint pain, swelling, and morning stiffness.
Psoriasis is a chronic inflammatory skin condition that causes red, thick, scaly patches, often accompanied by itching. While psoriasis can affect any part of the body, it most commonly appears on the knees, elbows, trunk, or scalp.
Both psoriatic arthritis and psoriasis are autoimmune diseases, meaning the immune system mistakenly attacks healthy cells in the body. Up to 40% of people with psoriasis develop psoriatic arthritis, though psoriasis itself is not contagious.
Causes
The exact cause of psoriatic arthritis is still unknown. Researchers believe it develops due to a combination of genetic and environmental factors. Problems with the immune system, infections, obesity, and physical trauma may also play a role in the onset of the disease.
Recent studies have shown that people with psoriatic arthritis have elevated levels of tumor necrosis factor (TNF) in the joints and skin affected by psoriasis. This increase can lead to immune system malfunction, affecting the body's inflammatory response.
Risk Factor
Several factors can increase the risk of developing psoriatic arthritis, including:
- Psoriasis
- Having psoriasis is one of the biggest risk factors for developing psoriatic arthritis.
- Family history
- If you have a parent or sibling with psoriatic arthritis, you may also be at higher risk.
- Age
- While psoriatic arthritis can occur at any age, it most commonly affects adults between 30 and 55 years old.
Symptoms
The severity of psoriatic arthritis symptoms varies from person to person. Some may experience mild symptoms affecting only one or two joints, while others may have more severe symptoms involving multiple joints.
Symptoms can flare up and worsen (relapse) or improve (remission) unpredictably, but proper treatment can help manage them. Common symptoms include:
- Fatigue
- Joint pain, stiffness, and swelling in one or two joints
- Swelling in fingers or toes, making them look like sausages (dactylitis)
- Reduced range of motion in affected joints
- Morning joint stiffness
Several common symptoms of psoriatic arthritis include:
Common joint symptoms:
- Pain and swelling in one or more joints, often in the hands, feet, ankles, or knees
- Stiffness, particularly in the morning or after sitting for long periods
- Limited range of motion in joints
- Pain or stiffness in the spine
- Swelling of tendons, such as the Achilles tendon, which attaches to the heel
- Swelling in the entire finger or toe (dactylitis)
Common skin symptoms:
- Red, thick patches with silvery or grayish scales
- Small scaly patches
- Thickened or pitted nails
- Nails separating from the nail bed
Other symptoms:
- Eye inflammation (iritis or uveitis)
- Fatigue
- Anemia
Read more: Anemia - Definition, Cause, Symptom, and Management
Diagnosis
Diagnosing psoriatic arthritis typically requires more than one examination. The doctor will assess your medical history, conduct a physical examination, and use blood tests and imaging studies to confirm the diagnosis.
Physical examination
The doctor will:
- Check joints for swelling or tenderness
- Examine fingers and toes for swelling or abnormalities
- Press on the soles of your feet or heels to check for pain
Imaging tests
- X-rays
- It helps assess changes in joint structure related to psoriatic arthritis
- MRI
- This examination uses radio waves that can produce clearer images of organs or tissues. MRI can be used to detect problems in the legs or lower back.
Laboratory tests
- Rheumatoid Factor (RF)
- RF is an antibody that is often detected in the blood of people with rheumatoid arthritis. This examination is used to rule out the diagnosis of rheumatism because in psoriatic arthritis, RF is not identified.
- Joint fluid test
- A needle is used to extract fluid from an affected joint, typically the knee. If crystals are found, gout may be the cause instead of psoriatic arthritis
- HLA-B27 test
- A blood test that helps diagnose psoriatic arthritis, especially if there is a family history of the disease
- ESR and CRP tests
- These blood tests can indicate inflammation levels in the body
Read more: Rheumatoid Arthritis - Definition, Cause, Symptom, and Management
Management
The primary goals of treating psoriatic arthritis are to relieve symptoms, prevent disease progression, and improve the patient's quality of life. Treatment options include:
- Medications:
- NSAIDs (Nonsteroidal anti-inflammatory drugs): To reduce pain and inflammation
- Corticosteroids: To reduce joint swelling and pain, which may be injected into the joint in cases of severe inflammation
- DMARDs (Disease-modifying antirheumatic drugs): These drugs block chemicals released when the immune system attacks joints, slowing the disease’s progression
- Physiotherapy
- Physiotherapy can reduce joint pain, allowing you to be more comfortable in your daily activities.
- Surgery
- Joint replacement surgery may be recommended by your doctor if the joint has been severely damaged and medication or physical therapy cannot relieve symptoms. The joint will be replaced with an artificial joint made of plastic or metal.
Complications
In a small population, psoriatic arthritis can progress to arthritis mutilans. Arthritis mutilans is a more severe form of psoriatic arthritis.
Over time, arthritis mutilans can destroy the small bones in the hand, especially the fingers. This can lead to permanent deformity and disability of the fingers.
Psoriatic arthritis can also increase the risk of developing hypertension, metabolic syndrome, high cholesterol, diabetes, and heart disease.
Prevention
Psoriatic arthritis cannot be prevented, but symptom progression can be managed by adopting healthy lifestyle changes, such as:
- Protecting your joints, for example, by using knee pads during physical activities or avoiding joint injuries
- Exercising regularly
- Maintaining a healthy weight
- Quitting smoking
- Reducing alcohol intake
When to See a Doctor?
If you have psoriasis and begin to experience joint pain, consult your doctor. Psoriatic arthritis can damage joint tissue if left untreated or treated. Early treatment can prevent joint damage and improve quality of life.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Psoriatic Arthritis. (2021). Retrieved 15 November 2022, from https://www.mayoclinic.org/diseases-conditions/psoriatic-arthritis/symptoms-causes/syc-20354076#:
Psoriatic Arthritis. (2019). Retrieved 15 November 2022, from https://www.nhs.uk/conditions/psoriatic-arthritis/#:
About Psoriatic Arthritis. (2022). Retrieved 15 November 2022, from https://www.psoriasis.org/about-psoriatic-arthritis/
What is Psoriatic Arthritis?. (2022). Retrieved 15 November 2022, from https://www.psoriasis.org/about-psoriatic-arthritis/
Psoriatic Arthritis. (2022). Retrieved 15 November 2022, from https://www.webmd.com/arthritis/psoriatic-arthritis/psoriatic-arthritis-the-basics
Psoriatic Arthritis. (2019). Retrieved 15 November 2022, from https://my.clevelandclinic.org/health/diseases/13286-psoriatic-arthritis#symptoms-and-causes
Psoriatic Arthritis. (2022). Retrieved 15 November 2022, from https://medlineplus.gov/psoriaticarthritis.html


/669f34947bb6a.jpg)