Definition
Hypogonadism, or gonadal deficiency, is a condition where the body is unable to produce sufficient sex hormones. In men, hypogonadism is characterized by decreased levels of testosterone. In women, it is marked by low levels of estrogen and progesterone. When hypogonadism occurs during adolescence, it may manifest as delayed puberty.
In both men and women, sex hormones are produced by the gonads. In men, the gonads are located in the testes, while in women, they are in the ovaries. These sex hormones serve functions such as:
- Regulating the development of breasts in women and testes in men
- Controlling the growth of pubic hair
- Playing a role in the menstrual cycle and sperm production, among other functions
There are two types of hypogonadism:
- Primary Hypogonadism
Primary hypogonadism occurs when the gonads are unable to produce adequate sex hormones due to issues within the gonads themselves. The gonads can still receive messages and signals from the brain, but they are incapable of producing the hormones.
- Secondary/Central Hypogonadism
In secondary or central hypogonadism, the problem lies in the brain. The hypothalamus and pituitary gland, which regulate the gonads to produce sex hormones, are not functioning properly.
Causes
The exact causes of hypogonadism are not fully understood. Primary hypogonadism, or issues with the gonads, is suspected to arise from several conditions, including:
- Certain autoimmune diseases are where the immune system attacks healthy cells
- Genetic disorders such as Klinefelter syndrome or Turner syndrome, where individuals are born with chromosomal abnormalities
- Severe infections of the testes
- Disorders of the kidneys or liver
- Exposure to radiation or chemotherapy
- Surgical procedures involving the testes or ovaries
Secondary hypogonadism may be caused by:
- Genetic disorders such as Kallmann syndrome, characterized by delayed or absent puberty
- Infections like HIV or tuberculosis
- Pituitary gland disorders
- Obesity or drastic weight loss
- Nutritional deficiencies
- Brain surgery
- Radiation exposure
- Injuries to the pituitary gland or hypothalamus
- Use of steroids and opioids
Risk Factor
It is normal for both men and women to experience a decline in sex hormones in their 40s or 50s, which can result in reduced sexual desire. The following factors may increase the risk of developing hypogonadism:
Primary Hypogonadism
- Endocrine and adrenal disorders such as:
- Diabetes mellitus, characterized by elevated blood sugar due to insufficient insulin production or poor insulin response
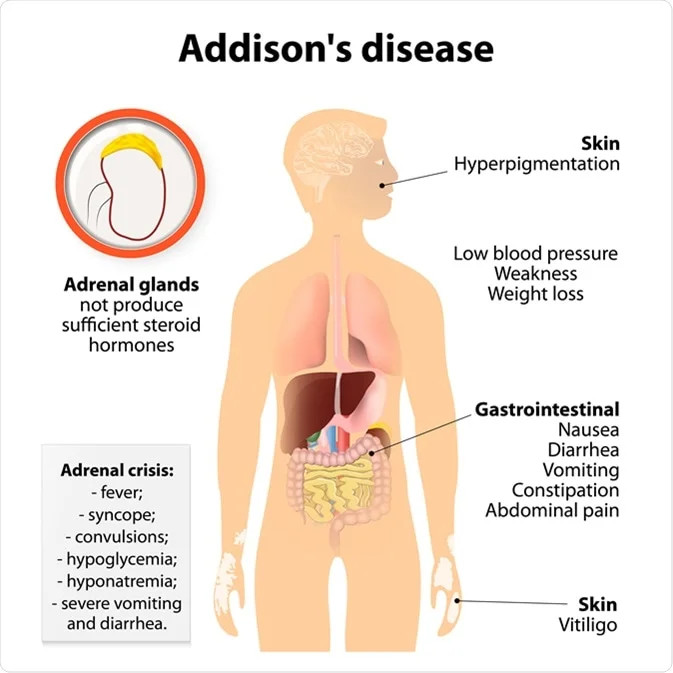
- Addison's disease, where the adrenal glands do not produce enough hormones
- Cancer treatments such as radiation and chemotherapy
- Genetic or chromosomal abnormalities such as Turner syndrome or Klinefelter syndrome
- Iron overload, known as hemochromatosis
- Kidney or liver disorders
- History of reproductive organ surgery
Secondary Hypogonadism
- Use of steroids or opioids
- History of brain surgery
- Cancer treatments
- Genetic disorders affecting brain development, such as Prader-Willi syndrome
- Tumors or disorders of the pituitary gland in the brain
Symptoms
Symptoms of hypogonadism vary depending on the cause and gender. Adolescents may be diagnosed with secondary hypogonadism if they do not experience puberty. For example, if a female does not get her first period or does not exhibit puberty signs such as breast development despite being of age, she may have hypogonadism. For male adolescents, signs include a lack of facial hair growth or undeveloped testes.
In adults, hypogonadism may present with sexual dysfunction, including:
- Decreased libido
- Loss of underarm and pubic hair
- Hot flashes (a warming sensation in the face, neck, and chest)
- Fatigue
- Difficulty concentrating
- Irregular menstrual cycles
- Abnormal discharge from the breasts
- Enlarged breasts in men (gynecomastia)
- Erectile dysfunction
- Reduced size of the penis and testes
- Decreased muscle mass
Diagnosis
Medical Interview
The doctor will start by asking:
- The patient's condition
- Main complaints and associated symptoms
- Past medical history
- Previous treatments
- Family medical history
- Daily activities
Physical Examination
The doctor will perform a general examination to check blood pressure, breathing rate, pulse, and body temperature. They will then assess puberty signs, especially in adolescents. For adult women, a pelvic examination may be conducted if necessary.
Diagnostic Tests
Diagnostic tests may include blood tests to measure sex hormone levels, thyroid hormones, and iron levels.
Radiological examinations, such as ultrasound, may be performed if conditions like polycystic ovary syndrome or ovarian cysts are suspected in women. Imaging studies such as MRI or CT scans may be used to check for tumors in the pituitary gland.
For men, sperm analysis might be necessary to measure sperm count.
Management
Treatment for hypogonadism depends on the underlying cause and the patient's gender. If the issue is with the gonads' ability to produce sex hormones, treatment will focus on increasing hormone levels. Hormone therapy may be used to boost estrogen and progesterone levels in women and testosterone in men.
In cases of secondary hypogonadism, treatment will target the underlying medical condition. For example, if a tumor in the brain or pituitary gland is identified, surgery, radiation, or chemotherapy may be employed to address it.
Complications
Complications of hypogonadism may include:
- Depression and anxiety due to hormonal imbalance
- Osteoporosis, particularly in women
- Infertility
- Relationship issues due to decreased sexual desire
Additionally, complications may arise from treatment, such as an increased risk of uterine cancer, blood clots, and stroke in women undergoing hormone therapy. However, these risks are minimal when treatment is supervised by a specialist.
Prevention
Prevention can start during adolescence by monitoring the signs of puberty. Early education on the signs and symptoms of hypogonadism is also essential. Avoid obesity or excess weight by maintaining a balanced diet, avoiding overeating, and exercising regularly.
When to See a Doctor?
Consult a doctor if you notice a child has not started menstruating or is missing puberty signs. If you experience any of the symptoms mentioned above, seek medical advice for further evaluation.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Cleveland Clinic - Low Sex Drive (Hypogonadism). (2020). Retrieved 8 October 2022, from https://my.clevelandclinic.org/health/diseases/15216-low-sex-drive-hypogonadism.
Medscape - Hypogonadism. (2022). Retrieved 8 October 2022, from https://emedicine.medscape.com/article/922038-overview.
Healthline - Hypogonadism. (2018). Retrieved 8 OCtober 2022, from https://www.healthline.com/health/hypogonadism.