Definition
Breast milk production disorders occur when the amount of breast milk produced is insufficient to meet a baby's needs. Although many breastfeeding mothers worry about not producing enough milk to meet their baby's needs, low milk production is actually quite rare. Generally, a breastfeeding mother's body is capable of producing the amount of breast milk required by her baby, even if she is not aware of it.
The belief that milk production is decreasing can lead mothers to switch to formula feeding. This is concerning, as replacing breast milk with formula can increase the risk of infant mortality and morbidity, as well as shorten the interval between pregnancies.
However, there are conditions that can lead to breast milk production disorders, and it is important for mothers to be aware of them. In general, these issues are caused by hormonal imbalances and occur in about 5% of breastfeeding mothers.
Causes
There are several causes of insufficient breast milk production or ineffective breastfeeding, including:
- Impaired infant growth due to certain diseases. Some conditions, such as hypothyroidism, congenital heart disease, cleft lip, and neurological disorders, can affect a baby's ability to nurse effectively. This may result in breast milk not meeting the baby's needs.
- Primary causes of breast milk production disorders. This can occur due to conditions like breast hypoplasia (underdeveloped breast tissue), breast surgery (including nipple piercings), and severe illnesses such as postpartum hemorrhage with Sheehan's syndrome, infections, or hypertension.
- Secondary causes of breast milk production disorders. These occur when milk is not regularly or sufficiently expressed from the breasts. This problem can arise from poor breastfeeding practices, such as waiting too long for the first feeding after birth or breastfeeding too infrequently. Lack of confidence in the mother or the belief that milk production is decreasing can also contribute to this problem.
Risk Factors
Various factors can lead to decreased milk production during breastfeeding, such as:
- Baby factors
- Premature birth, low birth weight, and various diseases, such as cleft lip and congenital heart disease.
- Maternal factors
- Maternal health: Conditions like anemia, postpartum hemorrhage, and smoking.
- Insufficient breast gland tissue: Not producing enough milk.
- Delaying the first breastfeeding session: Waiting too long to breastfeed after birth.
- Introducing bottles or pacifiers too early: Introducing bottle-feeding or pacifiers too soon.
- Limiting breastfeeding sessions: Resulting in the baby not getting frequent feedings.
- Incorrect breastfeeding technique
- Mental health issues, such as postpartum depression
- Perceived decrease in milk production: This can occur due to a lack of knowledge about breastfeeding and baby behavior or improper breastfeeding practices.
- Pain during breastfeeding: This can occur due to sore nipples from improper breastfeeding techniques or certain medical conditions.
- Maternal obesity
Symptoms
Several signs indicate that a baby is not getting enough breast milk, including:
- Baby does not seem satisfied after feeding: After being fed, a baby should appear more relaxed and open their fists. If the baby cries intensely and sucks their hand after feeding, this may indicate hunger.
- Increased crying frequency
- Longer feeding times
- Poor weight gain. Less than 20 grams per day. The baby's weight may decrease more than 10% from their birth weight and not return to birth weight within the first two weeks of life.
- No urine output in 24 hours
- Decreased stool volume: Hard and dry stools.
- Signs of dehydration, such as fewer than 4–6 wet diapers per day or a dry diaper for 6 hours or more, dry mouth, and sunken eyes with few tears.
Diagnosis
To diagnose breast milk production disorders, your doctor will take a thorough medical history and may perform some laboratory tests. They may ask if the mother has certain medical conditions, a history of breast surgery, smokes, or has hormonal issues, such as Polycystic Ovarian Syndrome (PCOS).
The doctor may also inquire about the birth process, including whether the mother experienced heavy bleeding after delivery or retained placental tissue, as conditions like anemia and retained placenta can reduce milk production.
Additionally, the doctor may assess the baby's health, such as measuring the baby's weight, evaluating the degree of weight loss, and checking for signs of dehydration. If a specific medical condition is suspected in the mother, the doctor may request blood tests to assess the mother's hemoglobin levels or thyroid hormone levels.
An ultrasound examination may be performed to check for retained placental tissue in the uterus. Urine tests for the baby might be conducted to rule out a urinary tract infection, which could weaken the baby and hinder effective breastfeeding.
If no disease is found in the baby, but low weight is still a concern, the doctor may evaluate breastfeeding techniques to ensure they are correct. Incorrect breastfeeding techniques can prevent the baby from effectively consuming breast milk.
Management
To increase breast milk production, several steps can be taken, including:
- Breastfeed the baby as soon as possible after delivery: The baby should be breastfed within the first hour after birth. Waiting too long to start breastfeeding can reduce milk production.
- Breastfeed from both breasts.
- Breastfeed frequently: The baby should be fed 8–12 times per day, approximately every 2–3 hours.
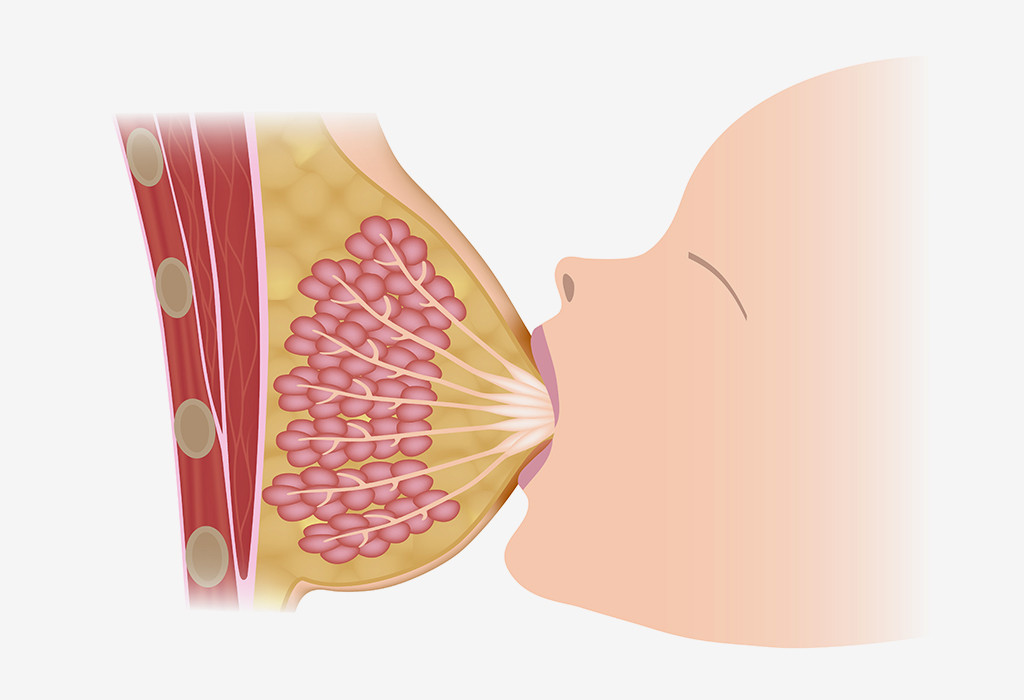
- Ensure proper breastfeeding technique: Correct techniques include: the baby's chin touching the mother's breast, the baby's mouth wide open, more of the upper areola visible than the lower areola, and slow, deep sucking by the baby.
- Avoid missing breastfeeding sessions: Pump breast milk if you miss a feeding to maintain milk production.
- Do not use pacifiers or bottles prematurely. If using a pacifier, wait until 3–4 weeks after birth.
- Be cautious with medications: Some medications, such as those containing pseudoephedrine (a cold medicine), can reduce milk production. Read more about pseudoephedrine here: [Pseudoephedrine - Mechanism, Contraindications, Side Effects].
- Avoid smoking and alcohol.
If these methods do not sufficiently increase milk production, your doctor may prescribe medications that can boost milk production. Substances or medications that promote milk production are called galactagogues. Common medications prescribed include domperidone, metoclopramide, or sulpiride.
Some plants are also known to increase milk production. Easily found in Indonesia are katuk leaves, moringa leaves, and torbangun leaves. Other natural substances that may help boost milk production include fenugreek, anise, fennel, cumin, grape, and coffee.
Complications
The primary complication of reduced milk production is failure to thrive. This can cause delays in various aspects of a baby's development, such as physical abilities (rolling over, sitting, standing, and walking) and mental and social skills.
Prevention
To prevent reduced milk production, there are several things mothers can do, including:
- Eat a balanced diet
- Drink enough fluids
- Get sufficient rest
- Avoid stress. Stress can inhibit the milk ejection reflex, leading to decreased milk production. To reduce stress, you can use relaxation techniques such as deep breathing, massage, eating and drinking your favorite foods, and listening to your favorite music. You also do not need to worry about how your breasts feel when touched. Your breasts will feel softer and less full as milk production adjusts to your baby's needs, so this does not mean that milk production is decreasing.
When to See a Doctor?
You should see a doctor if your baby shows signs of not getting enough breast milk, such as weight loss, frequent crying, or signs of dehydration, such as sunken eyes and fewer than 4–6 wet diapers a day. Mothers should also see a doctor if milk production decreases due to a medical condition they have, such as a history of breast surgery, hyperthyroidism, or anemia.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
WIC Breastfeeding Support USDA. (2022). Low Milk Supply. Retrieved 16 October 2022, from https://wicbreastfeeding.fns.usda.gov/low-milk-supply
Sultana, A., Rahman, K., & Manjula, S. (2013). Clinical Update and Treatment of Lactation Insufficiency. Medical Journal Of Islamic World Academy Of Sciences, 21(1), 19-28. doi: 10.12816/0000207
Mayo Clinic. (2022). Low milk supply: What causes it?. Retrieved 16 October 2022, from https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/expert-answers/low-milk-supply/faq-20058148
WIC Breastfeeing Support USDA. (2022). Baby's Hunger Cues. Retrieved 16 October 2022, from https://wicbreastfeeding.fns.usda.gov/babys-hunger-cues
Kent, J., Prime, D., & Garbin, C. (2012). Principles for Maintaining or Increasing Breast Milk Production. Journal Of Obstetric, Gynecologic &Amp; Neonatal Nursing, 41(1), 114-121. doi: 10.1111/j.1552-6909.2011.01313.x
Rizqi, L., Sutrisminah, E., & Adyani, K. (2022). Efektivitas Tanaman Lokal sebagai Galactagogue untuk Meningkatkan Produksi Air Susu Ibu. Jurnal Penelitian Kesehatan Suara Forikes, 13(1), 14-17. doi: http://dx.doi.org/10.33846/sf13103