Definition
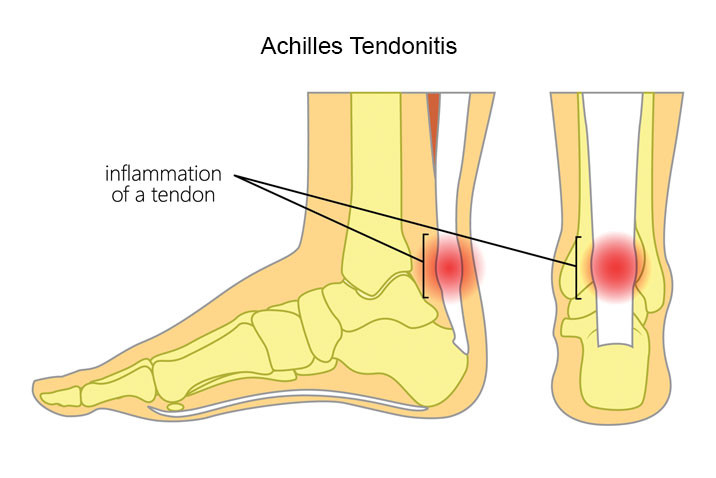
Achilles tendinitis is a condition that occurs when the Achilles tendon becomes irritated and inflamed. The Achilles tendon, the thickest and strongest tendon in the body, connects the calf muscles to the heel bone. It plays a crucial role in activities like walking, running, jumping, or standing on your toes.
Although the Achilles tendon can withstand significant stress during activities such as running and jumping, irritation can occur if the tendon is overused or subjected to excessive force. Achilles tendinitis refers to the irritation or inflammation that arises as a natural response to injury.
Achilles tendinitis differs from an Achilles tendon tear, in which the tendon separates from the heel bone or completely ruptures. However, in severe cases, the inflammation from Achilles tendinitis can lead to a tendon tear.
Causes
Achilles tendinitis is caused by repetitive or intense use of the Achilles tendon. This condition is common among runners who suddenly increase the intensity or duration of their runs. Rapidly increasing physical activity without allowing the body to adjust can trigger inflammation in the Achilles tendon.
The structure of the Achilles tendon deteriorates with age, making Achilles tendinitis common among middle-aged individuals who engage in weekend sports. Sudden stress on the Achilles tendon in such situations can cause irritation or inflammation.
Other causes of Achilles tendinitis include:
- Exercising without proper warm-up
- Tight calf muscles during repetitive movements
- Sports like tennis or basketball that involve sudden stops or directional changes
- Running too far, too intensely, or uphill too often
- Wearing high-heeled shoes daily or for long periods
Risk Factor
Several factors can increase the risk of Achilles tendinitis, including:
- Gender: Achilles tendinitis is more common in men than in women
- Age: The likelihood of Achilles tendinitis increases with age
- Physical abnormalities: Conditions like flat arches can place extra strain on the Achilles tendon
- Excess weight or obesity: This can put additional tension on the tendon
- Cold weather: Tendon pain tends to occur more often in cold climates
- Medical conditions: Conditions like psoriasis or high blood pressure are associated with a higher risk of Achilles tendinitis
- Certain antibiotics: Fluoroquinolones have been linked to an increased risk of Achilles tendinitis
Symptoms
The pain associated with Achilles tendinitis usually begins as mild discomfort in the back of the leg or above the heel after running or other sports activities. More intense pain can occur after prolonged running, climbing stairs, or sprinting. Stiffness or pain may also be more noticeable in the morning.
Other symptoms of Achilles tendinitis may include:
- Thickening of the Achilles tendon
- Swelling that worsens throughout the day or with activity
- Limited range of motion when flexing the foot
- Warmth around the heel or calf
Diagnosis
During a physical exam, your doctor will gently press on the painful area of your foot or heel to determine the exact location of the pain and whether there is tenderness or swelling. They will also assess the flexibility, range of motion, and reflexes of your foot and ankle.
Depending on the severity of the condition or if Achilles tendinitis is associated with other health problems, your doctor may recommend one or more diagnostic tests to assess the extent of the injury:
- X-rays
While X-rays cannot visualize soft tissues like tendons, they can help rule out other conditions that may cause similar symptoms.
- Ultrasound
This test uses sound waves to visualize soft tissues, including tendons. Ultrasound can also show the Achilles tendon moving in real time and may assess blood flow around the tendon.
- MRI
Magnetic resonance imaging uses strong magnets and radio waves to provide a detailed view of the Achilles tendon.
Management
Most cases of Achilles tendinitis can be treated with simple home care under a doctor’s guidance. Self-care strategies are important to prevent recurring episodes of Achilles tendon inflammation. The recommended method is the RICE method:
- Rest
Rest the affected leg for a few days. Avoid heavy activities to prevent putting undue stress on the Achilles tendon. In severe cases, a walking boot or crutches may be necessary.
- Ice
Apply ice packs to the back of the leg for 15 minutes after physical activity or when experiencing pain. This should be done during the initial days of the injury.
- Compression
Elastic bandages or wraps can help reduce pain and limit the tendon’s movement. Be careful not to wrap the area too tightly.
- Elevation
Elevate the injured leg above the level of the heart to reduce swelling. Sleeping with a pillow under the leg can help maintain elevation.
If symptoms are severe or persistent, your doctor may recommend additional treatments such as:
- Medications
If over-the-counter pain relievers like ibuprofen are insufficient, your doctor may prescribe stronger medications to reduce inflammation and relieve pain.
- Physical therapy
Your physical therapist may recommend the following treatment options:
-
- Therapists often provide a specific stretching and strengthening exercise plan to promote healing and strengthen the Achilles tendon and surrounding structures.
- Orthotics or shoe inserts that slightly elevate your heel can relieve pain in the tendon and provide cushioning that reduces the amount of pressure the Achilles tendon receives.
- Surgery
If nonsurgical treatments have been tried for several months without success, or if the tendon is torn, surgery may be necessary to repair the Achilles tendon.
Complications
Achilles tendinitis can weaken the tendon. In severe cases, the tendon may tear partially or fully, leading to reduced range of motion, difficulty walking, and potential scarring.
Prevention
Although Achilles tendinitis may not always be preventable, you can take several steps to reduce your risk:
- Exercise regimen
Gradually increase the duration and intensity of workouts rather than making sudden increases. Vary your exercise routine to avoid repeated stress on the same areas.
- Don't push yourself too hard
Avoid activities that place excessive stress on the tendon, such as running uphill. Warm up properly before engaging in intense activity. If you experience pain, stop and rest.
- Choose shoes carefully
Wear shoes that provide adequate cushioning and arch support to reduce strain on the Achilles tendon. Replace worn-out shoes, and consider arch supports if your shoes do not provide enough stability.
- Stretch daily
Regularly stretch your calf muscles and Achilles tendon in the morning, before and after exercise, to maintain flexibility.
- Strengthen your calf muscles
Strong calf muscles help the Achilles tendon handle the stress of physical activity more effectively.
When to See a Doctor?
If you experience persistent pain in your Achilles tendon, consult a doctor. Seek immediate medical attention if the pain is severe or disabling, as you may have torn your Achilles tendon.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Achilles tendinitis (2021) Mayo Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/achilles-tendinitis/symptoms-causes/syc-20369020 (Accessed: January 31, 2023).
Achilles tendinitis - orthoinfo - aaos (2022) OrthoInfo. Available at: https://orthoinfo.aaos.org/en/diseases--conditions/achilles-tendinitis/ (Accessed: January 31, 2023).
Badii, C. (2021) Achilles tendinitis: Treatment for heel pain and symptoms, Healthline. Healthline Media. Available at: https://www.healthline.com/health/achilles-tendinitis#What-is-Achilles-tendinitis? (Accessed: January 31, 2023).


/62c7b14af1315.jpg)






