Definition
Actinomycosis, also known as lumpy jaw or leptotrichosis, is a subacute or chronic bacterial infection caused by gram-positive, filamentous, anaerobic, and microaerophilic bacteria that are non-acid-fast. Actinomycosis typically causes abscesses in the soft tissues of the body, commonly occurring in the mouth, nose, throat, lungs, abdomen, and intestines. It rarely appears in other parts of the body but can spread from the initial infection site, leading to tissue damage.
Actinomycosis in humans was first discovered in 1857 by Lebert. In 1891, Wolff, an individual from Israel, successfully cultured the anaerobic bacteria Actinomyces israelii, the causative agent of the disease. With the widespread use of antibiotics, actinomycosis has become rare. Maintaining good hygiene, especially oral hygiene, is crucial. Actinomycosis is not contagious but can persist in the body for an extended period.
Causes
Actinomycosis is a rare infection in Indonesia. Initially thought to be caused by a fungus, it spreads slowly, but its true cause is bacterial, primarily from the family Actinomycetaceae. Several species are involved, including A. gerencseriae, A. viscosus, A. odontolyticus, Propionibacterium, and Bifidobacterium.
These bacteria naturally reside in body cavities like the nose and throat without causing infection unless they invade the body’s protective barriers. Actinomycosis can also occur due to gum disease.
Risk Factor
Actinomycosis is an infectious disease that causes inflammation. Factors that may increase your risk include:
- Being diagnosed with a compromised immunity. People with HIV/AIDS are more prone to infection
- Taking medications that can suppress the immune system. Long-term corticosteroids, for example, can suppress the human immune system and increase susceptibility to infection
- Malnutrition
- Trauma to the mouth or chin
- Dental abscesses
Read more: Dental Abscess—Definition, Cause, Symptom, and Treatment
Symptoms
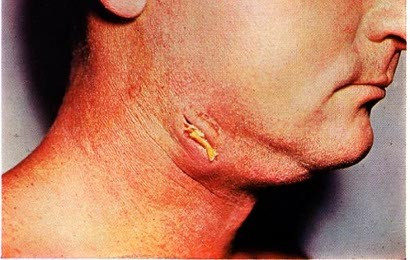
Actinomycosis often starts as an infection in the mouth, causing swelling in the jaw, which may feel hard and not painful initially. If an abscess develops, the swelling becomes red and painful. It can also cause muscle stiffness or lockjaw, limiting the ability to open the mouth normally.
Other symptoms may include:
- Fever
- Weight loss
- Swollen lumps on the neck and face
- Skin pain
- Cough
- Chest pain
Orocervical actinomycosis is the term for actinomycosis of the jaw. Jaw abscesses and lumps may result from this. Fifty percent of patients with actinomycosis experience jaw or orocervicofacial actinomycosis. Weakness, fever, phlegm-filled cough, and weight loss are the symptoms of actinomycosis, which can start in the chest cavity and spread to the lungs.
Actinomycosis in the digestive tract can cause abscesses, persistent fever, and diarrhea, and if it infects the stomach, it can spread to the heart. Actinomycosis symptoms include pelvic pain and vaginal discharge. Women with IUD contraception for more than 5-10 years are most commonly affected. Patients will also experience fever. Actinomycosis in the nerves can cause symptoms such as dizziness, brain abscesses, and permanent brain damage.
Diagnosis
Your doctor will ask about your symptoms and medical history, including any past dental surgeries or jaw infections. After a medical interview, a physical examination will be conducted to identify possible issues.
The following tests may be recommended:
- KOH Test. A 10% KOH preparation can help with diagnosis, usually with Gram staining.
- Histopathology. This test examines the tissue for fungal elements.
- Culture: Bacteria like Actinomyces israelii can be cultured in anaerobic conditions (without oxygen).
- Blood Tests: Antibody testing can help rule out other conditions. Blood cultures may detect systemic actinomycosis.
- Radiology: A CT scan or MRI of the jaw and chest may be used to detect bone damage, while abdominal radiology can identify masses in the abdomen, liver, or spleen.
A CT scan may be advised to check for bone destruction, while MRI is useful for confirming the diagnosis and monitoring treatment response.
Management
Antibiotics are the primary treatment for actinomycosis, with high-dose penicillin commonly prescribed. If you are allergic to penicillin, alternative antibiotics include:
- Tetracycline
- Clindamycin
- Erythromycin
Treatment may last six months or longer. If you have skin issues or abscesses, surgical excision may be necessary.
Complications
Although actinomycosis is not contagious, it can persist in the body for a long time. Initially infecting soft tissues, it may spread to other areas, causing complications such as:
- Bone infection. In severe cases, infected bone may need to be removed.
- Meningitis. A sinus infection can lead to meningitis, causing neck stiffness, fever, and headaches.
- Brain abscess. If the infection spreads to the brain, it can cause cognitive decline or even death.
Prevention
Actinomycosis can be prevented by:
- Maintaining good oral hygiene, brushing your teeth twice daily for at least 2 minutes
- Avoiding excessive alcohol consumption
When to See a Doctor?
If you experience any of the symptoms mentioned above, it is essential to see a doctor promptly. Early treatment leads to a better prognosis, and you should not stop taking antibiotics without your doctor’s approval.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
FK UI. Parasitologi kedokteran. 2016
Brazier, vincent. Medical News Today. What you should know about actinomycosis. 2018
Sampson, stacy. Healthline. Actinomycosis. 2022