Definition
A hemangioma is a bright red bump that appears at birth or in early life. It is formed by extra blood vessels, and the bump is benign. Hemangiomas typically grow for a while before disappearing on their own without treatment.
Causes
A skin hemangioma forms when blood vessel cells divide excessively in one area of the body. The exact cause of this abnormal division is unknown, but it is suspected that a protein produced by the placenta during pregnancy may be responsible. Hemangiomas can develop from the skin or the subcutaneous fat layer underneath. Initially, a hemangioma may appear as a red birthmark that grows into a lump. Hemangiomas are rarely present at birth.
Meanwhile, liver hemangiomas form on the surface of the liver. They may or may not be associated with skin hemangiomas that occur in infancy. If unrelated to infantile hemangiomas, the cause of liver hemangiomas is thought to be related to estrogen. Estrogen, a dominant sex hormone in females, is often prescribed during menopause to alleviate symptoms caused by decreasing estrogen levels. However, excess estrogen can promote the growth of liver hemangiomas. Similar to hormone replacement therapy, pregnancy and the use of birth control pills may enlarge hemangiomas.
Risk Factor
Hemangiomas are most common in premature female babies with fair skin. They also occur more frequently in babies born with low birth weight or who experienced oxygen deprivation before birth. Other risk factors include advanced maternal age, twin pregnancies, and genetic factors.
Symptoms
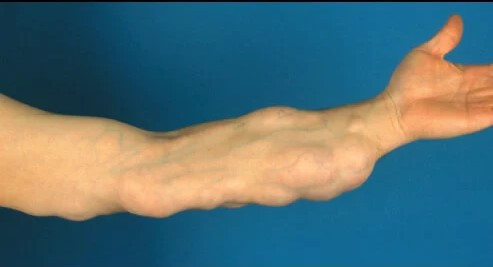
Hemangiomas can be present at birth, but they usually appear when a baby is a few months old. They typically start as bright red spots on certain areas of the body, most commonly the face, head, chest, or back. Usually, a child has only one hemangioma, but multiple hemangiomas can occur, especially in twins.
In the first year, the red spots grow quickly into soft, elastic lumps. Over time, the size stabilizes, and the hemangioma slowly fades. Most hemangiomas disappear by age five, and nearly all vanish by age ten. The skin where the hemangioma was may remain slightly discolored or raised.
If a hemangioma develops on an internal organ, symptoms will vary depending on its location. For example, a gastrointestinal hemangioma may cause:
- Nausea
- Vomiting
- Abdominal discomfort
- Loss of appetite
- Feeling full quickly
Diagnosis
Hemangiomas are usually diagnosed through observation. A skin biopsy may be performed if the doctor needs to confirm the diagnosis. Imaging tests such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) can assess the depth of the hemangioma and distinguish it from other tumors. Imaging is also used to detect hemangiomas in internal organs like the liver, kidneys, colon, and brain.
Management
Most hemangiomas do not require treatment, as they tend to disappear on their own. Treatment is prioritized for hemangiomas that cause complications or appear in sensitive areas, such as the lips. Treatment options include medications, laser therapy, and surgery. Care may involve specialists in pediatrics, dermatology, ophthalmology, and other fields, depending on the associated symptoms.
Medications
Medications for hemangioma treatment include beta blockers, corticosteroids, and gels. Beta blockers can be taken orally, but they may cause side effects such as slow heart rate, low blood pressure, bronchospasm, and low blood sugar. Corticosteroids can be injected, and if given in high doses, the dosage needs to be tapered over weeks to months. Side effects may include irritability, sleep disturbances, high blood pressure, bone loss, heart muscle damage, and growth problems. Bekaplermin gel is another option, though it is not yet available in Indonesia and has a potential cancer risk with repeated use.
Laser Therapy
Laser therapy can destroy hemangiomas on the skin. In some cases, doctors use lasers to reduce redness and improve appearance.
Surgery
Surgery is used for small hemangiomas, often removing the underlying fat layer. Internal organ hemangiomas may also require surgery. If the hemangioma is in the liver, blood flow to the tumor may be cut off.
Complications
Hemangioma complications may include:
- Wound, particularly in sensitive areas like the genitals, lower lip, armpits, and neck
- Vision problems such as amblyopia (lazy eye), astigmatism (irregular corneal curvature), farsightedness, nerve involvement, and blocked tear ducts
- Airway obstruction in the nose, under the vocal cords, or throat
- Feeding difficulties if the hemangioma is near the lips
- Multiple hemangiomas (multifocal), which may involve the liver and gastrointestinal tract
- Cosmetic concerns, especially for large hemangiomas on the face, nose (Cyrano nose), ears, or mouth
- PHACES syndrome when a facial hemangioma is larger than 5 cm and associated with vascular, heart, eye, and gastrointestinal issues
- LUMBAR syndrome if a hemangioma occurs on the spine, in the lower back region, and is linked to urinary, nerve, bone, vascular, and kidney problems
Most hemangiomas have a good prognosis. Around 50% disappear by age 5, 70% by age 7, and 90% by age 9. About 8% leave behind marks that may require treatment for cosmetic reasons.
Prevention
Preventing hemangiomas is difficult due to their uncertain cause, and most cases occur randomly. However, complications can be reduced by shrinking the hemangioma using medications, laser therapy, or surgery. Preventing cosmetic issues is important, as they can impact a child’s psychosocial well-being and that of their family.
When to See a Doctor?
Hemangiomas are usually visible and can be identified during routine checkups. However, you should consult a doctor if there are concerns about the hemangioma, such as bleeding, ulceration, or signs of infection. You should also seek medical advice if the hemangioma interferes with your child’s vision, breathing, hearing, or eating.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Chamli, A., Aggarwal, P., Jamil, R., & Litaiem, N. (2022). Hemangioma. Retrieved 15 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK538232/
Hemangioma - Symptoms and causes. (2021). Retrieved 15 April 2022, from https://www.mayoclinic.org/diseases-conditions/hemangioma/symptoms-causes/syc-20352334
Kahn, A., & Kramer, O. (2019). Hemangioma. Retrieved 15 April 2022, from https://www.healthline.com/health/hemangioma