Definition
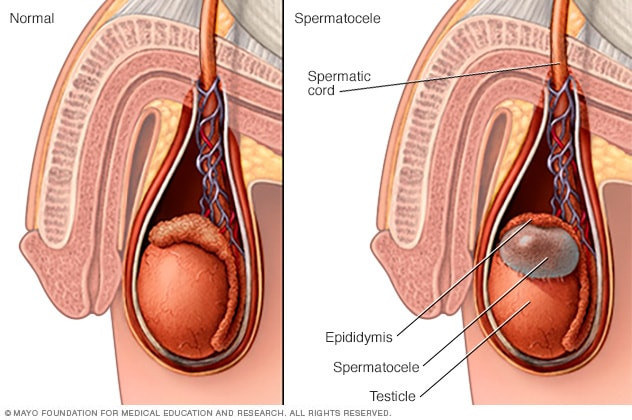
A spermatocele, also known as a sperm cyst, is an abnormal sac that forms in the epididymis, a small tube located at the top of the testicle. This tube is responsible for storing and transporting sperm. The cyst forms in the upper area behind the testicle but is separate from the testicle itself. Spermatoceles are benign and typically contain clear, cloudy, or milky fluid, which may also include sperm. In most cases, spermatoceles do not affect fertility or require treatment.
Causes
The male reproductive system is responsible for the production, maturation, and transportation of sperm. Disorders in this system can cause lumps to form, including spermatoceles. The exact cause of spermatocele formation remains unknown, but it is believed to result from a blockage in one of the epididymal ducts, which are responsible for channeling and storing sperm from the testicles.
Risk Factor
There are a few known factors that can increase the risk of developing a spermatocele. Men whose mothers were exposed to the drug Diethylstilbestrol (DES) during pregnancy to prevent miscarriage or other pregnancy complications may be at higher risk. The use of DES was discontinued in 1971 due to concerns about the drug’s link to rare vaginal cancer in women.
Symptoms
Spermatoceles typically do not cause any noticeable symptoms and may remain the same size over time. However, if a spermatocele enlarges, the following symptoms may occur:
-
A dull ache or discomfort in the affected testicle.
-
A feeling of heaviness in the testicle that contains the spermatocele.
-
A sensation of fullness behind and above the testicle.
Diagnosis
To diagnose a spermatocele, your doctor will begin by conducting a physical test. Although a spermatocele is generally painless, you may feel some discomfort during the examination. Additional tests may include:
-
Transillumination: This test involves shining a light through the scrotum. In the case of spermatoceles, the light will show that the lump is filled with fluid, not solid matter.
-
Ultrasonography (USG): If transillumination does not reveal a cyst, an ultrasound may be used to identify other potential causes. Ultrasound uses high-frequency sound waves to create images of the internal structure and can help rule out testicular tumors or other causes of scrotal swelling.
Management
Most spermatoceles do not require treatment as they typically do not cause pain, discomfort, or complications. However, if the spermatocele is large or painful enough to cause discomfort, over-the-counter pain relievers such as acetaminophen or ibuprofen may be recommended. Since spermatoceles usually do not shrink or go away on their own, the following treatment options are available:
- Surgery: A spermatocelectomy is typically performed as an outpatient procedure, using either local or general anesthesia. During this procedure, an incision is made in the scrotum, and the spermatocele is separated from the epididymis. After surgery, the doctor may advise you to:
-
Apply a cold compress to the scrotum for two to three days to reduce swelling. Swelling is common after surgery and may last from 2 to 21 days.
-
Take painkillers for one or two days following the procedure.
-
Wait 48 hours before taking a shower.
-
Return for a follow-up check-up in one to three weeks.
-
Although side effects from surgery are rare, they may include fever, infection, scrotal bleeding, and persistent pain.
- Aspiration with or without sclerotherapy: Another treatment option is aspiration and sclerotherapy, although these are rarely used. In aspiration, a special needle is inserted into the spermatocele to remove fluid. If the spermatocele reoccurs, your doctor may recommend a second aspiration followed by the injection of a chemical irritant into the spermatocele sac. This procedure is called sclerotherapy.
Complications
Spermatoceles generally do not lead to complications. However, the treatment procedure may cause damage to the epididymis or vas deferens. Such damage can negatively affect fertility. Another potential complication after surgery is the recurrence of the spermatocele, though this happens in only 10 out of 25 cases.
Because of the risk of fertility damage, the procedure is often delayed until you no longer wish to have children. If the spermatocele is causing severe discomfort and you prefer not to delay the procedure, it is advisable to discuss with your doctor the option of storing sperm in a sperm bank, along with the associated risks and benefits.
Prevention
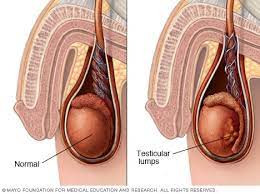
Although spermatoceles cannot be prevented, performing a self-examination of the scrotum at least once a month is essential to monitor for changes, such as lumps. Any new lump found in the scrotum should be promptly evaluated by a doctor. Your doctor can guide you on how to properly perform a self-examination of your testicles, which increases the likelihood of detecting a lump early.
The best time to examine your testicles is during or after a warm bath or shower, as the warmth relaxes the scrotum, making abnormalities easier to detect. To examine your scrotum, follow these steps:
-
Stand in front of a mirror and check for any swelling in the skin of the scrotum.
-
Use both hands to examine each testicle. Place your index and middle fingers under the testicle, and your thumbs on top.
-
Gently roll the testicle between your thumbs and fingers. Testicles are typically soft, oval, and firm. It is normal for one testicle to be slightly larger than the other. The epididymis, a tube running from the top of the testicle, is also a normal part of the scrotum.
By performing these checks regularly, you will become more familiar with the normal texture and size of your testicles, allowing you to spot any changes that may need medical attention. If you notice any unusual changes, such as lumps, swelling, or alterations in consistency, contact your doctor immediately.
Regular self-examination is an important aspect of maintaining good health, but it should not replace professional medical evaluations. Your doctor will usually check your testicles during physical exams.
When to See a Doctor?
A spermatocele is often found during a routine physical or self-testicular exam. If you detect any lumps in your scrotum, always consult a doctor to rule out more serious conditions, such as testicular cancer. You should also see a doctor if you experience pain or swelling in the scrotum. Several conditions can cause testicular pain, some of which may require immediate attention.
Looking for more information about other diseases? Click here!
- dr Hanifa Rahma
Spermatocele - Symptoms and causes. (2022). Retrieved 1 September 2022, from https://www.mayoclinic.org/diseases-conditions/spermatocele/symptoms-causes/syc-20377829.
Spermatoceles: Symptoms, Diagnosis & Treatment - Urology Care Foundation. Retrieved 1 September 2022, from https://www.urologyhealth.org/urology-a-z/s/spermatoceles.
Spermatocele: Symptoms, Causes, Treatments. (2020). Retrieved 1 September 2022, from https://my.clevelandclinic.org/health/diseases/17492-spermatocele.