Definition
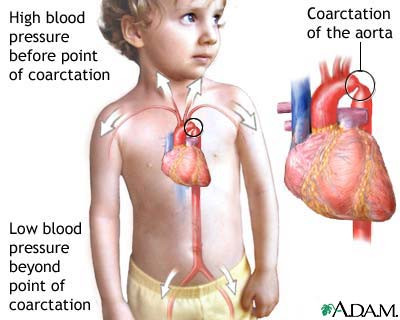
Coarctation of the aorta is a congenital condition where there is a narrowing of the aorta, the largest artery in your body, which carries oxygen-rich blood from the left ventricle of the heart to the rest of the body. This narrowing can occur anywhere along the aorta but is most commonly found in the juxtaductal aorta, the part near the ductus arteriosus, a short segment where the aorta arches downward toward the blood vessels branching into the chest and abdomen.
Coarctation of the aorta forces the heart to work harder to pump blood through the narrowed section of the aorta. Symptoms of coarctation of the aorta can vary from mild to severe. If the narrowing is severe and goes undiagnosed, serious complications may arise. Patients may require surgery or other procedures shortly after birth. Therefore, coarctation of the aorta is often considered a critical congenital heart defect. However, it may go undetected until adulthood, depending on the severity of the narrowing. Coarctation of the aorta is often associated with other heart defects.
Causes
Coarctation of the aorta is a congenital heart defect present at birth. The exact cause is not well understood. Some babies may develop heart defects due to genetic changes. In some cases, coarctation of the aorta develops later in life. Several conditions or factors that can narrow the aorta and lead to coarctation include:
- Injury
- Fatty plaque buildup that narrows the arteries (atherosclerosis)
- Rare types of artery inflammation (Takayasu’s arteritis)
Coarctation of the aorta usually occurs in the area after the upper branches of the aorta and before the lower branches. It often causes high blood pressure in your arms but low blood pressure in your legs and ankles. The left ventricle of your heart will work harder to pump blood through the narrowed aorta, leading to increased pressure in the left ventricle, which can cause its walls to enlarge and thicken.
Risk Factor
Male gender is more commonly affected by coarctation of the aorta than females. Additionally, certain genetic conditions, such as Turner syndrome (a disorder of the X chromosome in females), can increase the risk of coarctation of the aorta.
Other heart defects that may increase the risk of coarctation include:
1. Bicuspid Aortic Valve
The aortic valve separates the left ventricle from the aorta. A normal aortic valve has three flaps, but a bicuspid aortic valve has only two.
2. Subaortic Stenosis
This occurs when a thin membrane of tissue forms beneath the aortic valve, obstructing blood flow from the left ventricle to the aorta.
3. Patent Ductus Arteriosus
The ductus arteriosus is a blood vessel that connects the pulmonary artery (which connects the right ventricle to the lungs) to the aorta in babies. It allows blood to bypass the lungs while the baby is in the womb. Normally, it closes after birth, but if it remains open, this condition is called patent ductus arteriosus.
4. Atrial or Ventricular Septal Defects
Some babies are born with congenital heart defects where there is a hole in the wall separating the two atria (atrial septal defect) or the two ventricles (ventricular septal defect). This causes oxygen-rich blood from the left side of the heart to mix with oxygen-poor blood from the right side.
5. Congenital Mitral Valve Stenosis
The mitral valve, located between the left atrium and left ventricle, allows blood to flow through the left side of your heart. When this valve is narrowed, blood flow between the atrium and ventricle is reduced, increasing pressure in the left atrium. This increased pressure can cause fluid buildup in the lungs, leading to shortness of breath, which may occur during exercise or even when lying down.
Symptoms
Symptoms of coarctation of the aorta vary depending on the severity of the condition and the amount of blood able to flow through the aorta. Many people have no symptoms and may not be diagnosed until adulthood. Babies with severe coarctation may develop symptoms soon after birth, including:
- Pale skin
- Irritability
- Heavy sweating
- Difficulty breathing
- Feeding difficulties
Symptoms of coarctation in older children and adults include:
- High blood pressure
- Throbbing headaches
- Muscle weakness
- Leg cramps
- Cold legs
- Nosebleeds
- Chest pain
- Dizziness or fainting
- Decreased ability to exercise
- Poor growth
- Shortness of breath
Coarctation of the aorta may also occur alongside other heart defects, contributing to additional symptoms.
Diagnosis
Coarctation of the aorta is often diagnosed after a baby is born, and the timing of diagnosis depends on the severity of symptoms. Newborn screening with pulse oximetry in the first few days of life can help detect coarctation. In more serious cases, early signs like pale skin, irritability, heavy sweating, and difficulty breathing may prompt further evaluation.
Physical examination often reveals weaker pulses in the legs or groin compared to the arms or neck, and a heart murmur (abnormal heart sound caused by disrupted blood flow) may be detected with a stethoscope. Blood pressure in the arms and legs will also be measured, with higher pressure typically observed in the arms. Older children and adults with coarctation often have high blood pressure in the arms compared to the legs.
In addition to symptoms and physical examination, an echocardiogram, a type of ultrasound for the heart, is commonly used to confirm the diagnosis. It can show the structure of the heart, blood flow through the aorta, and how well the heart is functioning. Other tests, such as chest X-rays, electrocardiograms (ECG), MRIs, and cardiac catheterization, may also be used.
Management
The primary treatment for coarctation of the aorta involves widening the narrowed section of the aorta through:
1. Balloon Angioplasty
This procedure uses a thin, flexible tube called a catheter, which is inserted into the blood vessel and guided toward the aorta. Once the catheter reaches the narrowed area, a balloon at the tip inflates to widen the vessel. Sometimes a stent (a small tube) is inserted to keep the vessel open.
2. Surgery
During surgery, the narrowed section of the aorta is removed, and the aorta is reconstructed or patched to allow normal blood flow.
Complications
- Brain aneurysm
- Brain hemorrhage
- Aortic dissection
- Aortic aneurysm
- Heart failure
- Premature coronary artery disease, causing heart attacks before age 45
- Stroke
- Kidney failure
Prevention
Coarctation of the aorta cannot be prevented, as it is usually a congenital condition present at birth. However, early detection can reduce the risk of complications if you or your child have conditions that increase the risk of coarctation, such as Turner syndrome, bicuspid aortic valve, other heart defects, or a family history of congenital heart disease.
When to See a Doctor?
If a baby is born with the symptoms mentioned earlier, a doctor will typically perform further examinations. Routine blood pressure checks are recommended for early detection for both you and your child.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
CDC. Facts About Coarctation of the Aorta. (2022). Retrieved 11 April 2022, from https://www.cdc.gov/ncbddd/heartdefects/coarctationofaorta.html
Chen, MA. Coarctation of the Aorta. (2019). Retrieved 11 April 2022, from https://medlineplus.gov/ency/article/000191.htm
Coarctation of the Aorta. (2020). Retrieved 11 April 2022, from https://www.mayoclinic.org/diseases-conditions/coarctation-of-the-aorta/symptoms-causes/syc-20352529
Law, MA., et al. Coarctation of the Aorta. (2021). Retrieved 11 April 2022, from https://www.ncbi.nlm.nih.gov/books/NBK430913/
Meyer, K. Coarctation of the Aorta. (2022). Retrieved 11 April 2022, from https://www.cincinnatichildrens.org/health/c/coarctation
Mhanna, C., et al. Coarctation of the Aorta. (2021). Retrieved 11 April 2022, from https://kidshealth.org/en/parents/coa.html


/6260ea0df2071.jpg)