Definition
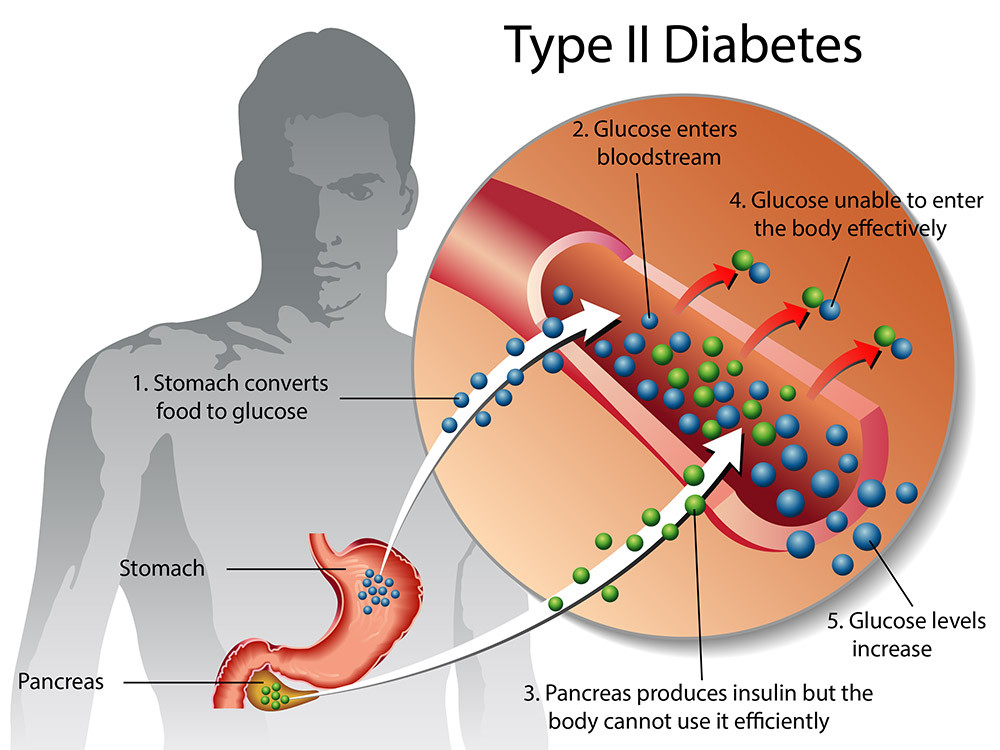
Type 2 diabetes mellitus (type 2 DM) is a disorder in which the body has difficulty regulating the use of glucose, or sugar, circulating in the blood as an energy source. In type 2 diabetes, the body's cells do not respond well to the hormone insulin, which prevents the sugar in the bloodstream from being used as an energy source. Insulin plays a role in regulating blood sugar levels in the body.
Additionally, due to the low levels of insulin circulating in the bloodstream, the pancreas, which is responsible for producing insulin, starts to produce less insulin. As a result, the amount of insulin available is not enough to meet the body's needs.
This chronic (long-term) condition results in too much sugar remaining in the blood, leading to one of the most common manifestations of diabetes: high blood sugar levels. Over time, this condition can cause problems in the circulatory system, nervous system, and immune system. Type 2 DM is more commonly found in middle-aged individuals over 45 years, although the number of cases is increasing among younger people with obesity.
If you are interested in reading further about diabetes in general, you can read it here.
Causes
In type 2 DM, glucose does not enter the cells but accumulates in the bloodstream. Type 2 DM is caused by two main interconnected problems:
- Cells in muscle tissue, fat, and the liver become resistant to insulin
Normally, when sugar circulates in the bloodstream, the pancreas receives a signal to produce insulin. This hormone helps transport sugar into cells, where it is then converted into an energy source. Glucose enters the cells, is converted into energy, and blood sugar levels decrease. When the pancreas detects low blood sugar, it reduces insulin production.
Cells need an energy source obtained from glucose, and the body's cells typically respond well to insulin. However, when these cells do not normally interact with insulin, sugar remains in the blood and is not transported into the cells. Therefore, the cells do not receive enough energy from the sugar circulating in the bloodstream, even though insulin is present.
- The pancreas cannot produce enough insulin
As blood sugar levels increase, the beta cells in the pancreas that produce insulin release more of it. Eventually, these cells can become damaged and unable to produce enough insulin to meet the high demand. Consequently, blood sugar remains elevated in the body.
Risk Factor
Factors that can increase the risk of type 2 diabetes include:
- Body weight
Being overweight or obese is a major risk factor for type 2 DM.
- Fat distribution
Accumulation of fat concentrated around the abdomen, as opposed to the hips and thighs, indicates a greater risk. The risk of type 2 DM increases if you are a man with a waist circumference over 100 cm or a woman with a waist circumference over 88 cm.
- Sedentary lifestyle
The less active you are, the higher your risk of type 2 DM. Physical activity helps control weight, uses glucose for energy, and makes cells more sensitive to insulin.
- Family history
The risk of type 2 DM increases if your parents or siblings have type 2 DM.
- Race and ethnicity
For reasons not yet fully understood, certain races and ethnicities have a higher likelihood of developing type 2 DM, including Black, Hispanic, Native American, and Asian individuals compared to White individuals.
- Blood lipid levels
An increased risk is also associated with low levels of HDL cholesterol ("good" cholesterol) and high levels of triglycerides (a type of fat).
- Age
The risk of type 2 DM increases with age, especially after 35-45 years.
- Prediabetes
Prediabetes is a condition where your blood sugar level is higher than normal but not high enough to be classified as diabetes. If untreated, prediabetes can develop into type 2 DM.
- Pregnancy-related risks
Your risk of developing type 2 DM increases if you have diabetes during pregnancy or if you give birth to a baby weighing more than 4 kg.
- Polycystic ovary syndrome (PCOS)
PCOS is a condition in women caused by an imbalance in reproductive hormones and is characterized by symptoms such as irregular menstrual cycles, excessive body hair growth, overweight, or acne. This condition can increase the risk of developing diabetes.
You can read more PCOS articles here.
Symptoms
Signs and symptoms of type 2 DM often develop slowly. You may even have type 2 DM for years without realizing it. Possible signs and symptoms include:
- Frequent thirst
- Frequent urination
- Increased hunger
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing wounds
- Frequent infections
- Tingling or numbness in hands or feet
- Darkened skin, usually in the armpits and neck
Diagnosis
In addition to medical interviews and physical examinations, type 2 DM is usually diagnosed using blood sugar tests and HbA1c tests. The HbA1c test measures the percentage of red blood cells bound with blood sugar over the past two to three months. The interpretation of the results is:
- Less than 5.7%: Normal
- 5.7% to 6.4%: Prediabetes
- 6.5% or more on two separate tests: Indicates diabetes
If HbA1c is not available or you have certain conditions affecting the test results, the doctor can use other tests to diagnose diabetes, such as:
- Random blood glucose test: A blood sugar level of 200 mg/dL or higher indicates diabetes, especially if you also have signs and symptoms of diabetes.
- Fasting blood sugar test: The interpretation of the results is:
- Less than 100 mg/dL: Normal
- 100 - 125 mg/dL: Prediabetes
- 126 mg/dL or higher: Diabetes
- Oral glucose tolerance test: This test is less commonly used except during pregnancy. You will fast overnight and then drink a sweet liquid provided by the doctor. Blood sugar will be tested periodically for two hours afterward. The interpretation of the results is:
- Less than 140 mg/dL: Normal
- 140 - 199 mg/dL: Prediabetes
- 200 mg/dL or higher after two hours: Indicates diabetes
Management
When diagnosed with type 2 diabetes mellitus, you need to change your lifestyle. Start by engaging in regular physical activity, adopting a healthier diet, and losing weight to reach the ideal range.
Your doctor will prescribe blood sugar-lowering medications or injectable insulin, which must be used or taken regularly. These medications help control blood sugar levels to stay within the normal range and prevent complications. You must regularly monitor your blood sugar levels. Your doctor may also monitor your blood pressure and cholesterol levels to ensure they remain within normal limits.
Complications
Common complications of diabetes and comorbidities include:
- Cardiovascular disease
Diabetes is associated with an increased risk of heart disease, stroke, high blood pressure, and narrowing of blood vessels.
- Peripheral nerve damage (neuropathy)
High blood sugar levels can damage nerves, causing tingling, numbness, burning, pain, or even loss of sensation, typically starting at the toes or fingers and gradually spreading upward.
- Other nerve damage
Nerve damage to the heart can cause irregular heart rhythms. Nerve damage in the digestive system can cause problems such as nausea, vomiting, diarrhea, or constipation. In men, nerve damage can also cause erectile dysfunction.
- Kidney disease
Diabetes can lead to chronic kidney disease or end-stage kidney disease, which may require dialysis or a kidney transplant.
- Eye damage
Diabetes increases the risk of serious eye conditions, such as cataracts and glaucoma, and can damage retinal blood vessels, potentially leading to blindness.
- Skin conditions
Diabetes can make you more susceptible to skin problems, such as bacterial and fungal infections.
- Slow healing
If untreated, wounds can develop serious infections, causing delayed healing. Severe damage may require amputation of toes, feet, or legs.
- Dementia
Type 2 DM appears to increase the risk of Alzheimer's disease and other conditions that cause dementia. Poor blood sugar control is associated with faster declines in memory and other cognitive abilities.
Prevention
A healthy lifestyle can help prevent type 2 DM. A healthy lifestyle includes:
- Healthy diet. Choose foods low in fat and calories and high in fiber. Focus on fruits, vegetables, and whole grains.
- Physical activity. Engage in moderate to vigorous aerobic activity regularly, such as brisk walking, cycling, running, or swimming, for at least 150 minutes per week.
- Weight loss. Losing weight and maintaining an ideal weight can slow the progression from prediabetes to type 2 DM. If you have prediabetes, losing 7 to 10 percent of your body weight can reduce the risk of diabetes.
When to See a Doctor?
You should see a doctor to monitor your health condition and identify any risk factors you may have.
Looking for more information about other diseases? Click here!
- dr. Alvidiani Agustina Damanik
Type 2 diabetes (2022) Mayo Clinic. Mayo Foundation for Medical Education and Research. Available at: https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193 (Accessed: December 13, 2022).
What is type 2 diabetes? (2020) NHS choices. NHS. Available at: https://www.nhs.uk/conditions/type-2-diabetes/ (Accessed: December 13, 2022).
Type 2 diabetes (2021) Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/diabetes/basics/type2.html (Accessed: December 13, 2022).